Excellent Info Site
 qap.ecdc.europa.eu
qap.ecdc.europa.eu
Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: this_feature_currently_requires_accessing_site_using_safari
More options
- Take 30 seconds to register your free account to access deals, post topics, and view exclusive content! Register TodayJoin the largest Oakley Forum on the web!You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.🦘Cacatman's Personal Coronavirus COVID-19 Update Thread
- Thread starter cacatman
- Start date
Diseases that REDUCE Risk of Complications of COVID-19
It appears that COVID-19 has a more favorable course in patients with congenital bleeding disorders; probably due to presence of a protective effect against COVID-19 related hypercoagulability.

(PDF) Do Congenital Bleeding Disorders Have a Protective Effect Against COVID-19? – A Prospective Study
PDF | Background: Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection is a grave clinical condition, with the most serious outcomes... | Find, read and cite all the research you need on ResearchGate www.researchgate.net Prevention - Melatonin?
www.researchgate.net Prevention - Melatonin?
Melatonin may reduce risk of getting COVID by 30%!
A network medicine approach to investigation and population-based validation of disease manifestations and drug repurposing for COVID-19
This study uses network medicine methodologies along with multiomic observations (including SARS-CoV-2 and human interactome, transcriptome, and proteome) to identify widespread disease manifestations and drug repurposing candidates (including melatonin) for COVID-19, validating these findings...journals.plos.org
“Melatonin may not directly promote the host defense system against the virus but increase the tolerance of the host to the virus,” Cheng explained. “In other words, in some aspect, to reduce the host defense system, for example, reducing the innate immune response and inflammatory reactions of the host.
https://www.lerner.ccf.org/news/details/?Cleveland+Clinic+Researchers+Use+“Big+Data”+Approach+to+Identify+Melatonin+as+Possible+COVID-19+Treatment&368b40ada56204bc8992942e8032bedb4d865564&390f8e37ac9d0069b5928b94dac2d4a31f491013
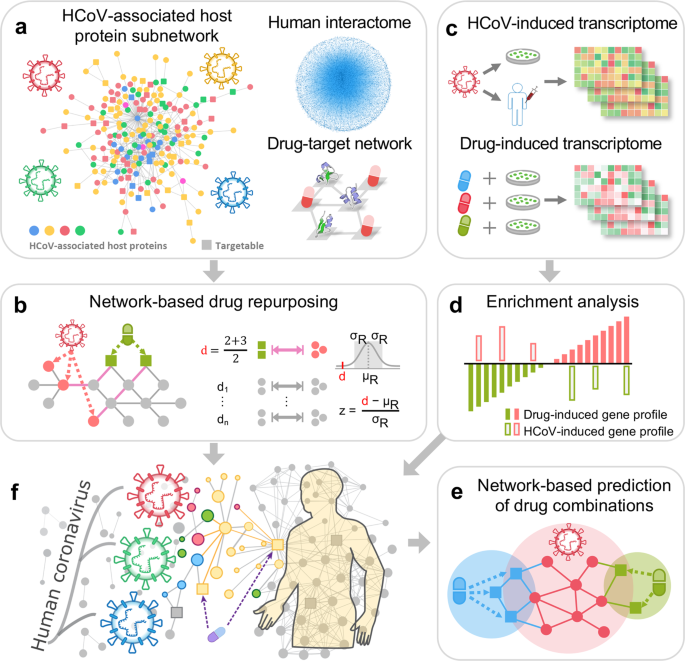
Network-based drug repurposing for novel coronavirus 2019-nCoV/SARS-CoV-2 - Cell Discovery
Human coronaviruses (HCoVs), including severe acute respiratory syndrome coronavirus (SARS-CoV) and 2019 novel coronavirus (2019-nCoV, also known as SARS-CoV-2), lead global epidemics with high morbidity and mortality. However, there are currently no effective drugs targeting... www.nature.com Last edited:Prognosis of Hospitalised Patients - All-comers
www.nature.com Last edited:Prognosis of Hospitalised Patients - All-comers
Here's an unpleasant stat. Of all patients ADMITTED to hospital for COVID, 30% had died in hospital or within 60 days of hospital discharge. An additional 15% of them were hospitalised again within 60 days. Half of the contacted patients reported emotional health being affected.
ACP Journals
www.acpjournals.org
14/12/20
In this national cohort of VA patients, 27% of survivors of COVID-19 hospitalization were readmitted or died by 60 days after discharge, and this rate was lower than matched survivors of pneumonia or heart failure. However, rates of readmission or death were higher than pneumonia or heart failure during the first 10 days after discharge following COVID-19 hospitalization, suggesting a period of heightened risk of clinical deterioration. Study limitations include the inability to measure readmissions to non-VA hospitals and an older, male-predominant study population, which may be at higher risk of severe manifestations of COVID-19. Public health surveillance or clinical trials focused exclusively on inpatient mortality may substantially underestimate burdens of COVID-19.

Readmission and Death After Initial Hospital Discharge Among Patients With COVID-19
This study describes reasons for readmission, use of ICU interventions during readmission, and proportions of death after initial hospital discharge of COVID-19 patients from US Veterans Affairs (VA) hospitals in March-June 2020. jamanetwork.com
jamanetwork.com
There were 2179 index hospitalizations for COVID-19, of which 678 patients (31.1%) were treated in an ICU, 279 (12.8%) were mechanically ventilated, 307 (14.1%) received vasopressors, and 1775 (81.5%) survived to discharge.
Within 60 days of discharge, 354 patients (19.9%) who survived COVID-19 hospitalization were readmitted, 162 (9.1%) died, and 479 (27.0%) were readmitted or died. Survivors with 60-day readmission or death were older, but otherwise similar to survivors without readmission or death (Table). Of those readmitted, the most common readmission diagnoses were COVID-19 (30.2%), sepsis (8.5%), pneumonia (3.1%), and heart failure (3.1%). During readmission, 22.6% were treated in intensive care, 7.1% were mechanically ventilated, and 7.9% received vasopressors. Index admissions totaled 27 496 hospital days, whereas readmissions after COVID-19 resulted in 3728 additional hospitalization days.

Readmission and Death After Initial Hospital Discharge Among Patients With COVID-19
This study describes reasons for readmission, use of ICU interventions during readmission, and proportions of death after initial hospital discharge of COVID-19 patients from US Veterans Affairs (VA) hospitals in March-June 2020. jamanetwork.com Last edited:This is probably one of the simplest explanations that communicates how small incremental changes can help keep you and others safe.
jamanetwork.com Last edited:This is probably one of the simplest explanations that communicates how small incremental changes can help keep you and others safe.
Every little bit counts!
Great GraphicZinc, Vitamin D, Vitamin C, NAC
Zinc
Zinc is known to be important for immune function. It has a role in antibody and white blood cell production and fights infections, while zinc deficiency increases inflammation and decreases the production of antibodies. High-dose zinc has also been found to reduce the duration of symptoms of the common cold. It is not yet clear whether zinc supplementation benefits patients with lower respiratory tract infections such as COVID-19. Because of its role in immune function and potential to decrease coronavirus replication, zinc is currently being investigated for the treatment of patients with COVID-19.
Vitamin D
Vitamin D deficiency is common, with lack of sun exposure, older age, corticosteroid use and darker skin associated with lower concentrations of 25-hydroxyvitamin D. This deficiency is associated with a higher incidence of acute respiratory infections. It is also hypothesized that there is a link between seasonal influenza and vitamin D deficiency. Vitamin D supplementation has also been shown to decrease the incidence of acute respiratory infection. While it has yet to be studied for prevention of COVID-19 infection and should not be recommended to patients, some recent articles have recommended taking daily supplements to raise 25-hydroxyvitamin D concentrations to reduce infection risk.
Vitamin C
Ascorbic acid, or vitamin C, is an antioxidant, with a number of studies suggesting that vitamin C supplementation impacts the immune system. Additionally, studies in birds have shown that vitamin C might protect against avian coronavirus infection, with human trials finding that vitamin C may decrease susceptibility to viral respiratory infections and pneumonia. New clinical trials are underway in China and the United States to determine if vitamin C might be used as a treatment for COVID-19.
N-acetylcysteine
N-acetylcysteine is converted to glutathione, which is an antioxidant that is depleted due to oxidative stress or systemic inflammation. Administration in vitro and in vivo leads to anti-inflammatory effects and antioxidant effects in a number of pulmonary diseases, including viral pneumonia and acute respiratory distress syndrome. Because patients with COVID-19 have evidence of systemic inflammation, often have their course complicated by acute respiratory distress syndrome, and may have respiratory mucus buildup limiting adequate airflow, systemic or aerosolized N-acetylcysteine (or both) may be beneficial in this specific patient population.
What is the role of supplementation with ascorbic acid, zinc, vitamin D, or N-acetylcysteine for prevention or treatment of COVID-19?
Several agents intended to supplement dietary intake or endogenous molecules may have a theoretical role in preventing or treating COVID-19. Because of their potential to influence immune response, ascorbic acid (vitamin C), zinc, vitamin D, and N -acetylcysteine have been hypothesized to be...www.ccjm.org
Differences in (Live) Viral Shedding Between Coronaviruses
79 studies (5340 individuals) on SARS-CoV-2, eight studies (1858 individuals) on SARS-CoV, and 11 studies (799 individuals) on MERS-CoV were included. Mean duration of SARS-CoV-2 RNA shedding was 17·0 days (95% CI 15·5–18·6; 43 studies, 3229 individuals) in upper respiratory tract, 14·6 days (9·3–20·0; seven studies, 260 individuals) in lower respiratory tract, 17·2 days (14·4–20·1; 13 studies, 586 individuals) in stool, and 16·6 days (3·6–29·7; two studies, 108 individuals) in serum samples. Maximum shedding duration was 83 days in the upper respiratory tract, 59 days in the lower respiratory tract, 126 days in stools, and 60 days in serum. Pooled mean SARS-CoV-2 shedding duration was positively associated with age (slope 0·304 [95% CI 0·115–0·493]; p=0·0016). No study detected live virus beyond day 9 of illness, despite persistently high viral loads, which were inferred from cycle threshold values. SARS-CoV-2 viral load in the upper respiratory tract appeared to peak in the first week of illness, whereas that of SARS-CoV peaked at days 10–14 and that of MERS-CoV peaked at days 7–10.
What I'd Do If I Had To Fly
You're actually much safer on a plane than in a room with someone. The air is recirculated 6-10 times an hour, so it's a lot better than in a normal environment. Studies have shown very little spread on planes because of the airflow.
- Try to get a window seat. You're less exposed to other people.
- Bring an extra mask or two. I'd also use a faceshield. I have one I can give you if you want. I'll send some photos. Some airlines want you to ALSO wear a faceshield.
- When in the airport/bathrooms, use an N95 mask. They're hard to breath in sometimes, so it may be uncomfortable for a long flight.
- Minimise going to the bathroom
- Turn the nozzle above you on maximum and aim it at your head. Wear a hat if you get cold easily.
- Try to avoid queuing for anything if possible ie. toilets
- Make sure you have enough hand sanitiser for the trip
- I'd bring antibacterial/viral wet wipes to wipe down your seat, especially arm rests and table/back of headrest.
- Request seat change if you notice someone coughing or not masking.
only problem is, nasal sprays are only to used in a very limited time period, 9 days max, or you might suffer damage and/or getting addicted to them. right, cacatman??Possible Nasal Sprays???!!!
?Nasal spray that blocks COVID-19? Novel, but I don't think this will work.

Nasal Spray Prevents Covid Infection in Ferrets, Study Finds (Published 2020)
Scientists at Columbia University have developed a treatment that blocks the virus in the nose and lungs, is inexpensive and needs no refrigeration.www.nytimes.com

